Introduction:
A chemical pregnancy, occurring within the first five weeks, can be an emotional and challenging experience. This article delves into the intricacies of chemical pregnancies, exploring their definition, causes, emotional impact, and how to cope with the aftermath. We also touch on risk factors, symptoms, and potential questions to ask your healthcare provider.
Defining Chemical Pregnancy:
A chemical pregnancy is essentially an early miscarriage that takes place within the initial five weeks of pregnancy. This occurs when the embryo starts developing but encounters obstacles, resulting in a halt in growth. Despite its early occurrence, the emotional impact can be significant, especially for those actively trying to conceive.
Causes and Timing:
Several factors, including genetic issues, hormonal imbalances, or structural challenges with the embryo, can contribute to a chemical pregnancy. It is unique in its timing, often happening so early that individuals might not even be aware they were pregnant. The article emphasizes the emotional toll, acknowledging that the experience varies from person to person.
Distinguishing Between Chemical and Clinical Pregnancy:
Explaining the difference between chemical and clinical pregnancies, the article highlights the significance of hormonal signals detected by pregnancy tests during the initial five weeks. It contrasts this with clinical pregnancies, where visible signs of fetal development appear on ultrasounds in later stages.
Reality of Miscarriage:
Addressing the reality of miscarriage, the article emphasizes that a chemical pregnancy is a valid and meaningful experience. Perception of the authenticity varies among individuals, and it explores how different people define the moment they consider the experience genuine.
Factors Affecting Miscarriage:
The article delves into factors that may increase the likelihood of miscarriage, including age, uterus shape, hormone levels, infections, and pre-existing health conditions. It emphasizes the importance of discussing potential risk factors with healthcare providers for personalized care plans.
Frequency and Indicators:
Discussing the frequency of chemical pregnancies, the article mentions that they make up around 25% of all pregnancies concluding before the 20-week mark. It also provides indicators, symptoms, and root causes, helping individuals identify and understand the signs of a chemical pregnancy.
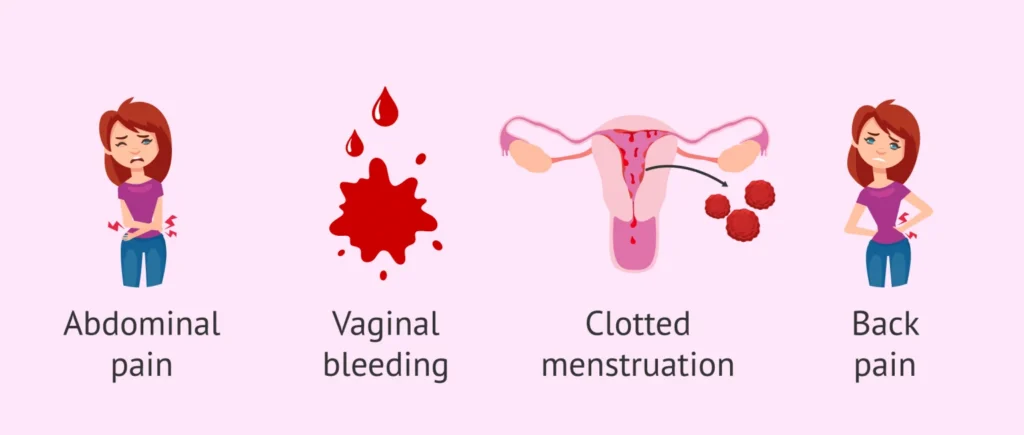
Bleeding in a Chemical Pregnancy:
The article explains the variations in bleeding during a chemical pregnancy, highlighting that it can differ from person to person. It covers the appearance, sensation, and potential outcomes of bleeding, providing a comprehensive understanding of this aspect.
Causes and Identification:
Exploring the causes behind a chemical pregnancy, the article delves into the role of hCG and the unknown factors leading to embryo development halting. It discusses how healthcare professionals identify chemical pregnancies through medical history and pregnancy tests.
Management and Treatment:
Addressing the management and treatment of chemical pregnancies, the article emphasizes that there isn’t a specific treatment. It reassures readers that many individuals who experience early pregnancy losses often go on to have successful pregnancies.
Avoiding Miscarriage:
While acknowledging that there isn’t a guaranteed method to prevent a chemical pregnancy, the article suggests maintaining overall reproductive health through regular check-ups, a balanced diet, and avoiding harmful substances. It highlights the importance of consulting healthcare professionals for personalized advice.
Moving Forward After Chemical Pregnancy:
Providing guidance for those wondering about the future after a chemical pregnancy, the article reassures individuals that having one doesn’t hinder their ability to conceive again. It encourages individuals to take time to process emotions and discuss next steps with partners or healthcare providers.
Ovulation After Chemical Pregnancy:
Addressing the timing of ovulation after a chemical pregnancy, the article suggests that it can occur approximately two weeks afterward, providing an opportunity for conception. It offers a hopeful perspective for those considering trying for another pregnancy.
Questions for Healthcare Provider:
The article lists questions individuals may want to ask their healthcare providers after experiencing a chemical pregnancy, covering topics like when to consult a fertility specialist, how long to wait before attempting to conceive again, lifestyle changes, and recommended tests.
Specialist Advice:
The article concludes by providing specialist advice, acknowledging the unpredictability of early pregnancies, and reinforcing the importance of self-care and seeking support from healthcare providers or counselors during this challenging time.
