Dive into the world of intrauterine insemination (IUI), a procedure that offers hope to couples trying to have a baby. In simple terms, it’s a method where doctors put concentrated sperm directly into the uterus when a woman is ovulating. This increases the chances of healthy sperm reaching the egg released by the ovaries.
Many couples seeking to get pregnant opt for IUI as a common fertility treatment. This detailed guide is here to give you the information you need to make informed decisions on your journey to starting a family.
What is Intrauterine Insemination (IUI)?
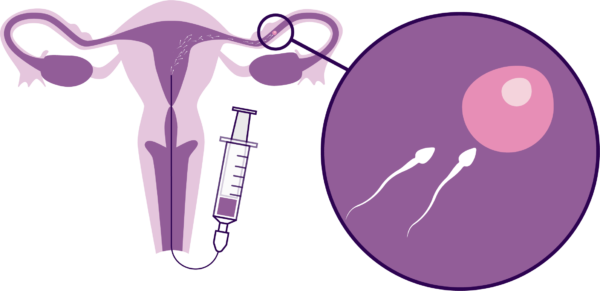
Intrauterine insemination (IUI) is a fertility treatment where sperm is carefully placed directly into a person’s uterus. Let’s understand why this matters for those trying to have a baby.
In a natural conception, sperm has a challenging journey from the vagina through the cervix, into the uterus, and finally to the fallopian tubes where the egg is released. Surprisingly, only 5% of sperm make this journey successfully. After the egg is released, it heads to the fallopian tube for potential fertilization.
With IUI, the sperm goes through a process of collection, washing, and concentration to keep only the high-quality ones. These selected sperm are then inserted directly into the uterus using a thin tube called a catheter. This method shortens the distance the sperm needs to travel and the time it takes, making it more likely to meet and fertilize the egg. This increases the chances of getting pregnant.
Healthcare providers often recommend IUI as an initial step before more invasive and costly fertility treatments. IUI can be done using sperm from your partner or a donor. Additionally, fertility drugs might be prescribed to ensure the release of eggs during ovulation, further enhancing the chances of successful conception.
Why do people opt for Intrauterine Insemination (IUI)?
IUI is performed to address various fertility challenges that couples may encounter. It is a recommended fertility treatment in situations such as cervical mucus issues or other cervix-related problems, low sperm count, abnormalities in sperm quality, difficulties with ejaculation or erection, semen allergies, and cases of unexplained infertility where the cause cannot be identified by healthcare providers. By strategically placing treated and concentrated sperm directly into the uterus during ovulation, IUI aims to optimize the chances of successful fertilization, offering a viable path to conception for those seeking assistance in building their families.
In detail, IUI might be recommended under the following circumstances:
Cervical Issues: If there are problems with cervical mucus or other cervical issues, IUI may be suggested. The cervix, the part that separates the vagina and uterus, produces mucus that aids sperm movement. Thick mucus can hinder sperm swimming, but IUI allows sperm to bypass the cervix and go directly to the uterus.
Sperm Problems: Low sperm count or abnormalities in sperm may necessitate IUI. Semen analysis during infertility evaluation might reveal issues like small, weak, slow, or misshapen sperm. IUI addresses this by selecting only high-quality sperm for the treatment.
Ejaculation or Erection Issues: IUI can assist when one partner faces challenges in getting or maintaining an erection or is unable to ejaculate.
Semen Allergy: In rare cases where individuals have an allergy to their partner’s semen, causing discomfort, IUI can be effective. The process of sperm washing during IUI removes the proteins triggering the allergy.
Unexplained Infertility: When healthcare providers cannot identify a specific cause for infertility, IUI may be recommended as a potential solution.
These varied scenarios showcase the versatility of IUI as a fertility treatment, tailored to address specific challenges that individuals or couples may encounter on their journey to parenthood.
How long does the IUI process take?
The entire IUI procedure typically spans about four weeks, roughly equivalent to a regular menstrual cycle, which is around 28 days.
Before starting the IUI journey, you and your partner will undergo a thorough examination, which may involve bloodwork, semen analysis, ultrasound, and other diagnostic tests. Depending on your situation, your healthcare provider might prescribe oral fertility medication for five days or injectable medication for up to two weeks. These medications aim to boost the chances of ovulation and the release of multiple eggs, although not everyone needs them.
The actual insemination process is swift, lasting only a few minutes as the sperm is inserted. Afterward, your healthcare provider might suggest lying down for about 15 minutes.
You can take a pregnancy test approximately two weeks after the insemination procedure to determine if it was successful
Can IUI help you get pregnant?
Well, the chances of success depend on what’s causing the difficulty in getting pregnant. IUI tends to work better for those with unexplained infertility or problems like cervical mucus or ejaculation issues. However, if the challenge is due to conditions like problems with fallopian tubes, endometriosis, or severe sperm issues, IUI might not be the most effective option. In such cases, treatments like IVF (in vitro fertilization) could be more suitable for improving the chances of pregnancy.
How does Intrauterine Insemination (IUI) differ from In Vitro Fertilization (IVF)?
The main distinction between IUI and IVF lies in where fertilization takes place. In IUI, fertilization happens inside your fallopian tube. First, a sperm sample is collected and purified, leaving only high-quality sperm. Then, this refined sample is introduced into your uterus using a catheter during ovulation. The goal is to make it easier for the sperm to reach the egg, increasing the chances of fertilization.
On the other hand, IVF involves fertilizing the egg with sperm outside of your body, typically in a laboratory setting. Once fertilized, the embryo is then placed into your uterus. In comparison to IVF, IUI is more affordable and involves fewer invasive procedures. However, it’s important to note that IUI tends to have a lower success rate per cycle when compared to IVF.
Procedure Breakdown
Curious about the steps involved in IUI treatment?
While specifics can vary between treatment plans and healthcare providers, the general process of IUI typically encompasses the following:
Ovulation Timing in IUI Treatment:
In the process of IUI treatment, accurate knowledge of your ovulation timing is paramount. This ensures that the injection of sperm aligns precisely with this crucial phase. Determining your ovulation time can be achieved through various methods. You may use an at-home ovulation prediction kit designed to identify luteinizing hormone (LH). Alternatively, healthcare providers can conduct blood tests to detect LH levels. Transvaginal ultrasound is another tool they may employ to observe indications of mature eggs. In certain cases, an injection of human chorionic gonadotropin (hCG) or other fertility medications may be administered to induce the release of one or more eggs. Typically, ovulation takes place approximately 10 to 16 days after the commencement of your menstrual cycle. The subsequent step of insemination, involving the introduction of sperm into your uterus, generally occurs within 24 to 36 hours after LH detection (either in blood or urine) or following the hCG injection.
Preparation of Semen Sample:
On the day of the IUI procedure, your partner contributes a freshly obtained sperm sample. Alternatively, in certain situations, your partner may provide the sample beforehand, and your healthcare provider can freeze it for later use. When utilizing sperm from a donor, the frozen sample is thawed and readied for the procedure.
The process of preparing sperm for insemination involves a technique known as “sperm washing.” This method extracts a concentrated quantity of healthy sperm, enhancing their viability for fertilization. In cases involving donor sperm, the sperm bank typically dispatches sperm that has already undergone the washing process.
Insemination Process Breakdown
The insemination procedure is a straightforward and brief process that typically only takes a few minutes. During this, you’ll be positioned on the examination table. Your healthcare provider will gently insert a speculum into your vagina, a routine akin to a Pap test. Subsequently, a catheter is carefully guided through your cervix into the uterus. At this point, the healthcare provider administers the washed sperm sample directly into your uterus.
Following the insemination, you may be advised to recline for a period of 10 to 30 minutes. The potential for pregnancy exists if the sperm successfully fertilizes an egg, and the resulting fertilized egg implants itself in the lining of your uterus.
In certain cases, your healthcare provider might recommend the use of progesterone post-IUI. Progesterone plays a role in sustaining the uterine lining, thereby enhancing the likelihood of successful implantation.
About two weeks after the IUI procedure, you have the option to take a pregnancy test. For a comprehensive understanding of the IUI process and what to anticipate, it is strongly advised to consult with your healthcare provider, who can provide tailored information based on your unique circumstances.
How should you get ready for IUI treatment?
Prior to commencing IUI treatment, thorough medical assessments and fertility tests are imperative. Both you and your partner will undergo examinations and various tests, which may involve:
1. Uterine Examination:
– A comprehensive evaluation of your uterus.
2. Uterus Ultrasounds:
– The use of ultrasounds to gather detailed information about the condition of your uterus.
3. Semen Analysis:
– Examination of your partner’s semen to assess its quality.
4. STI and Infectious Diseases Screening:
– Tests to screen for sexually transmitted infections (STIs) and other infectious diseases.
5. Blood Tests:
– Complete blood tests to analyze various aspects related to fertility and overall health.
Additionally, your healthcare provider may advise incorporating folic acid into your routine, typically found in most prenatal vitamins. This recommendation may begin at least three months before conception or the initiation of IUI treatment. This proactive approach aims to optimize your health and enhance the chances of a successful outcome. Always consult with your healthcare provider to tailor these preparations to your individual circumstances and needs.
What to Anticipate Post IUI Treatment:
Following intrauterine insemination (IUI), individuals may encounter mild symptoms, such as:
1. Mild Cramping:
– Expect some slight cramping, which is a common and generally temporary response to the procedure.
2. Spotting for a Day or Two:
– Spotting, or light vaginal bleeding, may occur for a brief period, typically lasting one or two days.
It’s common for most individuals to resume their normal activities immediately after IUI. While there are usually no specific restrictions, it’s advisable to avoid any activities that cause discomfort. Additionally, a pregnancy test can be taken approximately two weeks post-IUI to determine the success of the procedure. Always consult with your healthcare provider for personalized guidance and to address any concerns related to your specific situation.
Is IUI treatment painful?
IUI does not necessitate anesthesia, and the procedure itself is generally not painful. However, it’s common to experience mild cramping and discomfort during and immediately after the insemination process.
What medications are administered during IUI?
The integration of fertility medications with IUI is a common practice, intended to stimulate the ovaries for optimal egg production and release. While not universally necessary, this combined approach is often employed. Several medications may be employed, including:
1. Clomiphene Citrate (Clomid® or Serophene®): This medication is frequently used to induce ovulation by stimulating the ovaries to release eggs.
2. Letrozole (Femara®): Another option for promoting ovulation, Letrozole is employed to encourage the release of eggs.
3. hCG (Human Chorionic Gonadotropin): This hormone is administered to trigger the release of mature eggs from the ovaries, facilitating the subsequent steps of the IUI process.
4. FSH (Follicle-Stimulating Hormone): Fertility medications may also include FSH to encourage the development of follicles in the ovaries, supporting the production of eggs.
5. Prenatal Vitamins: Recommended for all pregnancies, prenatal vitamins are often advised during IUI treatment to ensure optimal nutritional support.
The decision to incorporate fertility drugs into your IUI treatment will be determined by your healthcare provider based on individual circumstances and needs.
What is the Expense Associated with IUI?
Determining the cost of Intrauterine Insemination (IUI) involves several factors, and it can vary based on the fertility clinic selected, your health background, and the inclusion of medications and diagnostic tests. Compared to other fertility treatments such as In Vitro Fertilization (IVF), IUI tends to be more cost-effective. The expenditure for a single IUI cycle typically ranges between $300 and $4,000 when not covered by insurance. It’s important to note that some states have regulations mandating insurance companies to contribute to covering a portion of the expenses related to infertility treatments.
What are the Potential Risks of IUI?
In comparison to more invasive fertility treatments such as IVF, IUI is generally considered low-risk. However, it’s important to be aware of potential risks associated with this procedure:
1. Multiple Births:
– Taking fertility medication to stimulate egg production may increase the likelihood of releasing more than one egg.
– This elevates the chances of conceiving twins, triplets, or even more.
– Multiple pregnancies carry a higher risk of premature labor and low birth weight for the babies.
2. Infection:
– While rare, there is a minimal risk of infection associated with the IUI procedure.
3. Spotting:
– Vaginal bleeding, though typically minimal, can occur as a result of the IUI procedure.
4. Ovarian Hyperstimulation Syndrome (OHSS):
– OHSS is a rare side effect linked to the excessive use of fertility medication.
– Symptoms include painful and swollen ovaries.
– It’s crucial to monitor medication dosage to minimize the risk of OHSS.
Being informed about these potential risks allows individuals undergoing IUI to make educated decisions and ensures that any concerns are addressed by healthcare providers. It’s essential to recognize that while these risks exist, they are generally infrequent in the context of intrauterine insemination.
What are the prevalent side effects associated with Intrauterine Insemination (IUI)?
Fertility medications, a common component of IUI treatment, may induce mild side effects in some individuals. Following insemination, the most frequently reported side effects include cramping and spotting.
Engaging in the IUI process can pose mental and physical challenges. Couples or individuals grappling with infertility issues and undergoing assisted reproductive technologies may find themselves contending with feelings of depression. If you’re experiencing disappointment or feeling overwhelmed during this journey, it is crucial to communicate with your healthcare provider. They can offer guidance and support to help you navigate the emotional and physical aspects of the IUI process effectively.
Recovery and Future Prospects
How effective is IUI in achieving pregnancy?
IUI can be quite effective, especially when fertility drugs are part of the process. When fertility drugs are used, the chance of pregnancy through IUI can go up to 20%. The effectiveness of IUI depends on the root cause of infertility and the age of the person trying to conceive. The success rate of IUI is comparable to natural conception, hovering around 20%, indicating that IUI boosts the chances to a more typical success rate.
How soon can you find out if you’re pregnant after IUI?
You’ll be able to determine if you’re pregnant approximately two weeks after IUI. It takes this amount of time for the pregnancy hormone, human chorionic gonadotropin (hCG), to be detectable in either blood or urine. Your healthcare provider will guide you on whether to come in for a blood test to confirm pregnancy or if you can use an at-home urine test.
How many rounds of IUI should you attempt before considering IVF?
Many healthcare providers suggest trying three cycles of IUI before exploring other reproductive options like IVF. For individuals over the age of 40, some healthcare providers may recommend moving on to IVF after just one cycle of IUI. This is because IVF tends to have higher success rates in this age group, and timely intervention is crucial.
In certain situations, bypassing IUI and opting for IVF directly might be more suitable. This is particularly true if you have conditions such as endometriosis, damage to the fallopian tubes, or advanced maternal age.
If pregnancy hasn’t occurred after three cycles of IUI, your healthcare provider will have a conversation with you about the next steps in your fertility journey.
When to Reach Out to Your Doctor
When should I get in touch with my healthcare provider during IUI treatment?
If you’re using fertility medications for IUI, it’s important to contact your healthcare provider if you experience any of the following:
1. Severe pelvic or abdominal pain.
2. Nausea and vomiting.
3. Shortness of breath.
4. Sudden weight gain.
5. Dizziness or lightheadedness.
Additional Insights
Is there anything I can do to boost my chances of getting pregnant with IUI?
Several factors influence the success of IUI, including age, the use of fertility drugs, overall health conditions, and the specific cause of infertility. Your healthcare provider will collaborate with you to identify strategies to enhance your chances of achieving pregnancy through IUI.
What is the success rate of IUI?
Apart from the cause of infertility, age plays a significant role in determining the success of IUI. Most healthcare providers recommend IUI before the age of 40 to improve the likelihood of pregnancy. The pregnancy rates for IUI by age are as follows:
– Age 20 to 30: 17.6%
– Age 31 to 35: 13.3%
– Age 36 to 38: 13.4%
– Age 39 to 40: 10.6%
– Over 40: 5.4%
Is IUI preferable to IVF?
Many individuals attempt IUI before opting for IVF due to its affordability and less invasive nature. However, in some cases, your healthcare provider may suggest IVF over IUI based on factors such as age or the underlying cause of infertility. Each treatment has its merits, and the choice depends on your specific circumstances and the likelihood of conception.
Can I engage in sexual activity after IUI?
Yes, you can have sex both before and after IUI. Having intercourse on the day of IUI or the following day can increase your chances of becoming pregnant.
Important Note: If you’re facing difficulties in conceiving, consult with your healthcare provider. Infertility is a common challenge, and various options, including IUI, may be available to assist you. Your healthcare provider will guide you in choosing the right fertility treatment to enhance your chances of a successful pregnancy.
